September 29th is World Heart Day. This special edition of The Evidence Speaks will highlight CHÉOS Scientist Brian Grunau’s (right) research on out-of-hospital cardiac arrests in Vancouver.
__
Barbic D, Klinkenberg B, Grunau B, Christenson J. Do neighbourhoods in Vancouver and surrounding areas demonstrate different rates of bystander CPR and survival for out-of-hospital cardiac arrest? CJEM. 2016 Oct 17. Epub ahead of print. doi:10.1017/cem.2016.384.
Out-of-hospital cardiac arrest is one of the leading causes of death in Canada, and the chances of surviving hospital treatment with a good neurological outcome lie between 8.2 and 10.4 per cent. CHÉOS Scientist Dr. Brian Grunau, an emergency physician at St. Paul’s Hospital, co-authored a study on the geographic distribution of out-of-hospital cardiac arrests in the southern part of the Vancouver Coastal Health region. The research looked for clusters and investigated how various variables—such as an area’s median income, demographics, and distance to the nearest hospital—correlate with the rates of bystander CPR and outcomes for the patients.
The investigators examined 1617 cases of out-of-hospital cardiac arrests, for which the mortality rate was 86.5 per cent. Forty-two per cent of cases received CPR from bystanders. Of those who were transported to the hospital by paramedics (49.7 per cent), 10.4 per cent were discharged with a favorable neurological status.
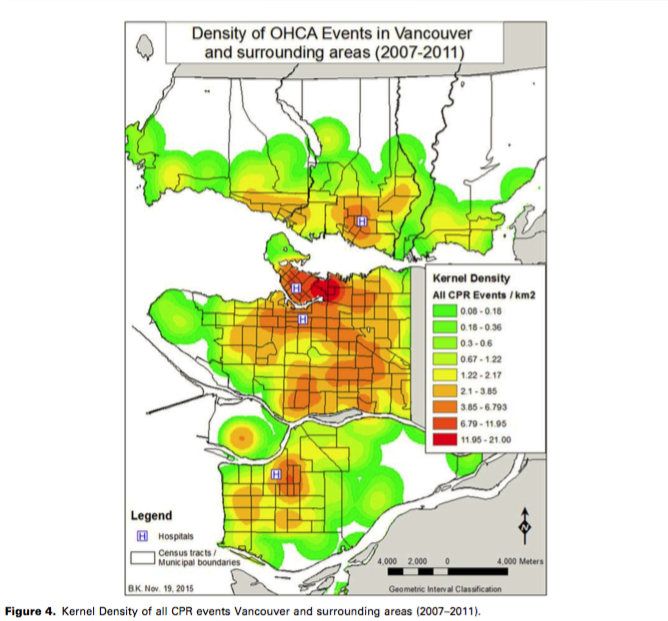
The authors found that the highest density of cardiac arrests had occurred in the downtown, Hastings, and Mount Pleasant neighborhoods. Overall, income was not linked to the geography of out-of-hospital cardiac arrests, but it correlated with the likelihood that a victim would receive CPR from a bystander in public or private.
There were fewer cases involving public bystander CPR than the authors anticipated in areas with a high median income. The rates of public bystander CPR were higher in areas with median income less than $21,000 and in neighborhoods with a greater number of recent migrants. Moreover, in areas with a high density of ethnic Chinese residents, the authors found that cardiac arrest victims were more likely to receive public bystander CPR relative to the rest of the study region.
The outcomes differed when the authors looked at the incidence of CPR in private, however. In places where fewer than 55 per cent of people held a postsecondary degree, victims of cardiac arrest were less likely to receive private CPR, and conversely, private CPR was more common in areas with high median incomes.
While income did not predict a survival with favourable neurological outcomes, when the distance of transport to hospital was less than 7.2 km, the patient’s chances of survival with favourable neurological outcomes were significantly higher.
This study can inform local public education efforts aiming to improve survival from out-of-hospital cardiac arrests by increasing the rates of bystander CPR.
—
Grunau B, Carrier S, Bashir J, Dick W, Harris L, Boone R, Kalla D, Scheuermeyer F, Twaites B, Straight R, et al. A comprehensive regional clinical and educational ECPR protocol decreases time to ECMO in patients with refractory out-of-hospital cardiac arrest. CJEM. 2017 Aug 16. Epub ahead of print.
Survival of out-of-hospital cardiac arrests treated by emergency medical services range from 3 to 16 per cent, but emerging data suggests that extracorporeal cardiopulmonary resuscitation (ECPR), a form of extracorporeal membrane oxygenation (ECMO) applied during cardiac arrest, may improve survival in younger, previously healthy victims of a sudden cardiac arrest, whose condition was quickly recognized and treated with prompt CPR. Positive outcomes appear to be strongly associated with the time from cardiac arrest to ECPR initiation, and if this time exceeds 75 minutes, survival is rare.
St. Paul’s Hospital had the capacity for ECPR but it was applied on case-by-case basis and the treatment was initiated slowly. Thus, Dr. Grunau and a team of clinicians developed a formal regional protocol for out-of-hospital cardiac arrests, which dictated pre-hospital and in-hospital steps for identifying and managing ECPR candidates. The intention of the protocol was to improve the rate of survival of out-of-hospital cardiac arrests with good neurological function among young and previously healthy patients by rapidly identifying ECPR candidates and minimizing the time from arrest to ECPR initiation, with the goal set at under 75 minutes.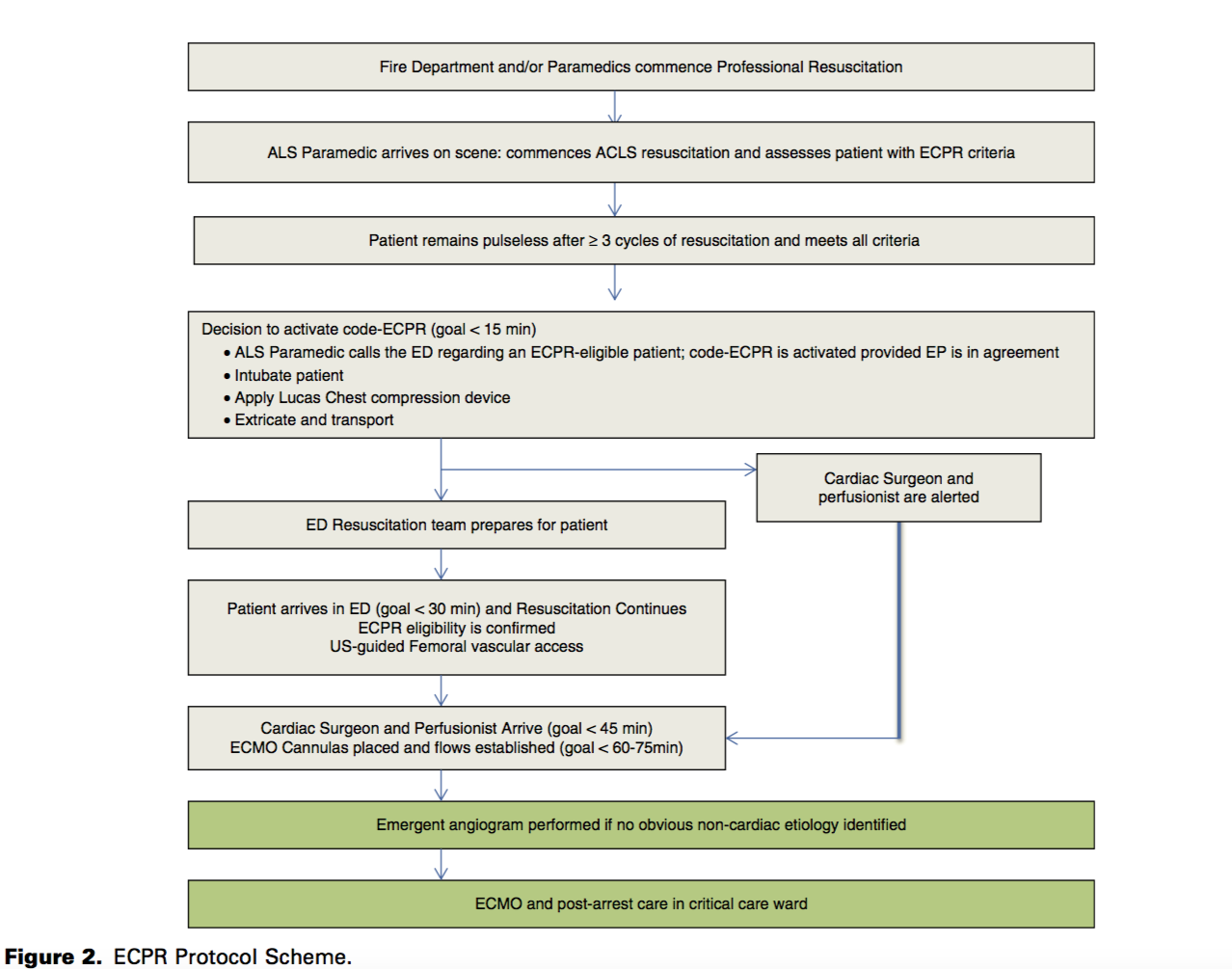
After the protocol was implemented, ECPR was attempted in nine patients, seven of whom had adequate ECMO flows established and two of whom survived. Both survivors were discharged with favourable neurological outcomes. The median time-to-ECPR was 60 minutes during the protocol period, reduced from 136 minutes prior to protocol implementation. Although the authors note that the study is unable to make conclusions about ECPR efficacy, the protocol for initiating ECPR for suitable patients improves the crucial timing of treatment, and can inform the development of similar protocols in other hospitals.



