For National Health Ethics Week, read about our newest Scientist, Dr. Anita Ho, and the unique approach she is taking to promoting ethical decision-making.
Dr. Anita Ho is an ethicist affiliated with the W. Maurice Young Centre for Applied Ethics (School of Population and Public Health) at UBC as an associate professor. Her research centers on the investigation of how and why patients and family members make health care decisions and how they can be supported in making ethically appropriate decisions in the context of their situation.
What began as a biomedical ethics elective during a marketing undergraduate degree quickly evolved into graduate training in philosophy, focused on understanding how people from different social and economic backgrounds perceive an accessible and equitable health care system. Throughout her career, Dr. Ho has consulted with clinicians and researchers to overcome ethical hurdles and to discuss best practices for ethical, shared decision-making.
During her time as an ethicist at PHC Ethics Services, Dr. Ho found that clinical decisions, such as “how do we discharge an elderly patient with no stable housing?” often required the consideration of the wider societal and systemic implications.
“Bedside ethics are important but it’s not enough to deal with problems one patient at a time,” said Dr. Ho. “If we can’t find ways to address ethical issues at a system level, we will be stuck doing the same thing over and over.”
This quandary impelled Dr. Ho to pursue a master’s degree in public health and a research program that focuses on the development of ethically sound policy, research design, and medical education. Her current program of research is focused on supportive and shared decision-making for various chronic conditions (e.g., heart failure, chronic kidney diseases, cancers) and end-of-life care decisions and explores best practices for the inclusion of patients and family members in decisions about their care and health care trajectory.

Supportive Decision-making for Diverse Populations
Supported by a CIHR operating grant from 2012 to 2015, Dr. Ho led a qualitative interview and focus group project to identify what care providers, patients, and family members found to be the most supportive aspects of their decision-making and what were some barriers to making decisions that were congruent with their values.
“The core concept behind this study was the need to promote patients’ self-determination and autonomy,” said Dr. Ho. “But health care is inherently relational. This called for the exploration of current decision-making process and the factors that either limit or promote supportive decision-making.”
The project included the use of interviews and focus groups with diverse patient groups (including Punjabi-speaking, Chinese-speaking, Farsi-speaking, and Aboriginal communities) and health care providers, in order to identify attitudes towards individual and system-wide barriers and facilitators related to decision-making. Specifically, the project explored decision-making in determining appropriate care plans in complex health care situations.
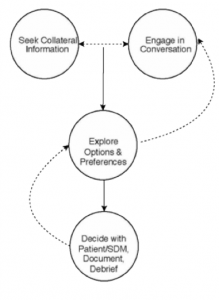 On top of expanding our understanding of the context in which decision are made, the project resulted in the development of the SEED (i.e., Seeking collateral information, Engaging in conversations, Exploring preferences and options, and Deciding with patients/families, debriefing, and documenting)modelof decision-making. [more about the SEED model here and here]
On top of expanding our understanding of the context in which decision are made, the project resulted in the development of the SEED (i.e., Seeking collateral information, Engaging in conversations, Exploring preferences and options, and Deciding with patients/families, debriefing, and documenting)modelof decision-making. [more about the SEED model here and here]
“The SEED model takes an interprofessional approach and can be used by clinicians who want to partner with patients to make person-centered decisions and to empower them,” noted Dr. Ho.
In collaboration with knowledge users, the SEED model was developed into a digital platform that can more fully guide clinicians through resources and steps that are customized to a particular patient’s goals and priorities.
“The digital format is more than just a decision aid, it acts as a communication, information-gathering and resource coordination tool,” she said. “The platform has a series of dynamic feedback loops that prepares people for decision-making and supports them in doing so.”
The model is adaptable to other care scenarios and conditions (e.g., medical assistance in dying (MAiD), elective orthopaedic surgeries) and the paper version is being used in studies in Tanzania, Rwanda, and South Korea. Dr. Ho is currently exploring the use of the digital version in heart failure (HF) care settings in Canada.
“Previous research suggests that almost 20% of heart failure patients who receive implantable cardioverter-defibrillators say that they didn’t want it,” said Dr. Ho. “Given the high-risk, resource-intensive nature of this procedure, we clearly need to involve this patient group in discussions about their care goals in the early stages of treatment.”
Dr. Ho is designing a study, with other CHÉOS Scientists Drs. Nick Bansback and Hubert Wong as co-investigators, to help health care providers better engage with HF patients and to assess whether the SEED model is effective, feasible, and acceptable to patients and providers.
“Use of this platform can help providers make decisions in collaboration with their patients that both parties are confident in, that minimize potential distress, and that are focused on patients’ goals and values,” she added.
Balancing Act
Dr. Ho splits her time between Vancouver and the University of California, San Francisco where she is an associate adjunct professor involved in global health research focused on ethical distribution of health care resources.
She is also involved in developing ethics education for health care students and spent three years as the Director of Ethics Curriculum at the Centre for Biomedical Ethics, National University of Singapore.
Other ongoing projects include an exploration of palliative and hospice care workers’ experiences in providing end-of-life care in the era of legalization of medical assistance in dying.



