The Evidence Speaks Series is a recurring feature highlighting the latest in CHÉOS research. This series features summaries of select publications and is designed to keep media and the research community up to date with CHÉOS’ current research results in the health outcomes field.
To ensure this research is quick and easy to share, we are now providing social cards that you are free to save and use as you see fit.
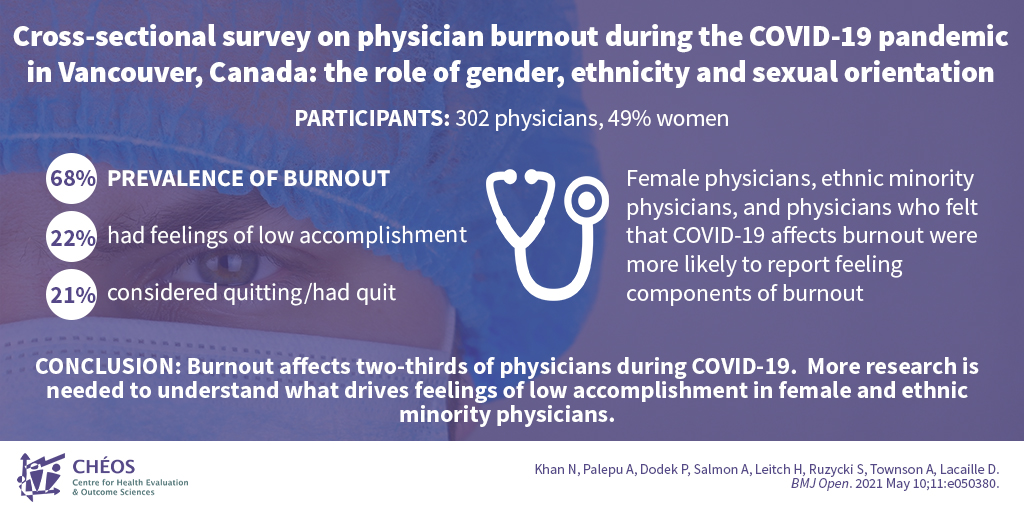
Survey indicates female and ethnic minority physicians may be more likely to experience burnout
Khan N, Palepu A, Dodek P, Salmon A, Leitch H, Ruzycki S, Townson A, Lacaille D. Cross-sectional survey on physician burnout during the COVID-19 pandemic in Vancouver, Canada: the role of gender, ethnicity and sexual orientation. BMJ Open. 2021 May 10;11:e050380.
In a study led by a team from CHÉOS, two-thirds of physicians reported experiencing burnout during the COVID-19 pandemic. Of the 302 respondents they surveyed, 22% also felt low personal accomplishment and 21% said they were considering quitting, or had already quit, their profession. Drs. Nadia Khan, Anita Palepu, Peter Dodek, and Amy Salmon also wanted to determine the potential role of gender, ethnicity, and sexual orientation in physician burnout. Women, ethnic minorities, and those who felt that COVID-19 affects burnout were more likely to report feeling components of burnout than other physicians. The survey results indicated that interventions to reduce inefficient work practices and reduce non-physician work could be beneficial. Furthermore, interventions to improve feelings of personal accomplishment should be considered.
—
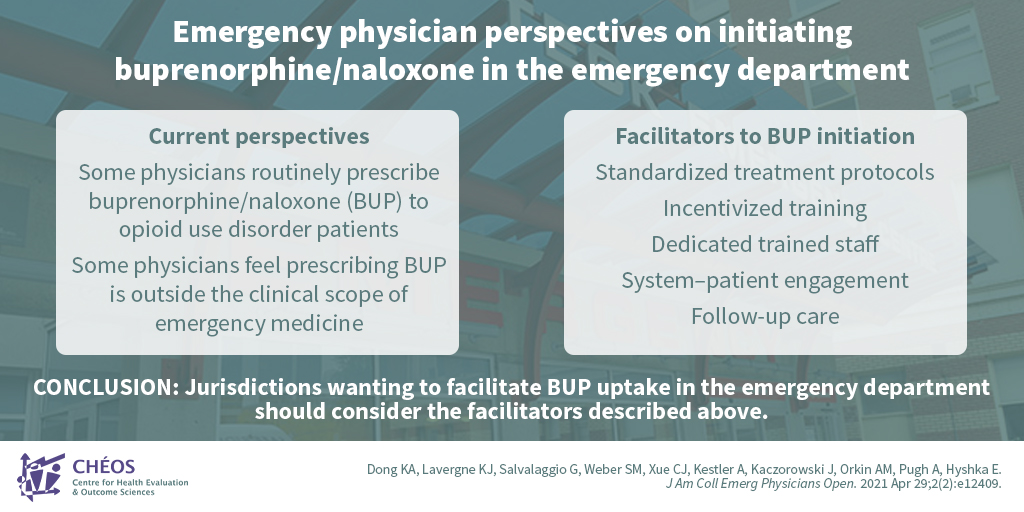
Researchers identify facilitators to initiating buprenorphine/naloxone for patients with opioid use disorder in the emergency department
Dong KA, Lavergne KJ, Salvalaggio G, Weber SM, Xue CJ, Kestler A, Kaczorowski J, Orkin AM, Pugh A, Hyshka E. Emergency physician perspectives on initiating buprenorphine/naloxone in the emergency department: A qualitative study. J Am Coll Emerg Physicians Open. 2021 Apr 29;2(2):e12409.
CHÉOS Scientist Dr. Andrew Kestler joined researchers from across Canada to investigate the perspectives of emergency physicians on prescribing buprenorphine/naloxone (BUP) for patients with opioid use disorder in the emergency department (ED). BUP is a recommended first-line treatment for opioid use disorder. Among the 32 participating physicians, care of opioid use disorder patients in the ED varied, with some reporting that they routinely prescribed BUP and others stating that they believed this was outside the clinical scope of emergency medicine. The study showed that standardized treatment protocols, incentivized training, dedicated trained ED staff, system–patient engagement, and follow-up care were important facilitators for BUP initiation in the ED, and they should be considered in locations wanting to aid BUP uptake.
—
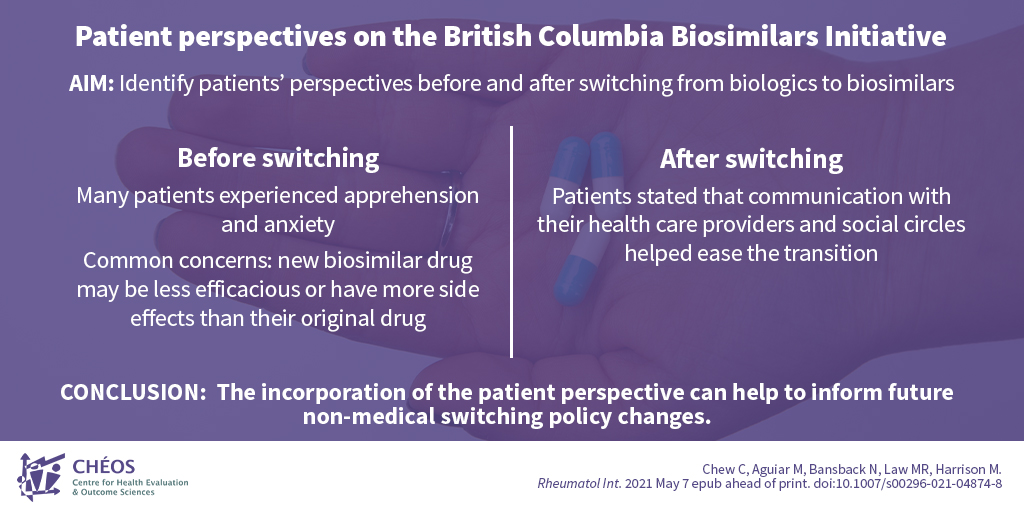
Patients switched to a biosimilar drug were helped with the transition through good communication
Chew C, Aguiar M, Bansback N, Law MR, Harrison M. Patient perspectives on the British Columbia Biosimilars Initiative: a qualitative descriptive study. Rheumatol Int. 2021 May 7 epub ahead of print. doi:10.1007/s00296-021-04874-8
A group of researchers from UBC, including CHÉOS Program Head of Decision Sciences Dr. Nick Bansback and Scientist Dr. Mark Harrison, recently conducted several interviews to determine patients’ perspectives of switching from biologic (originator) drugs to biosimilar versions following B.C.’s launch of the Biosimilars Initiative in 2019. Before switching to a biosimilar, many patient participants experienced apprehension and anxiety, with common concerns being that the new biosimilar drug may be less efficacious or have more side effects than their current drug. However, following the switch, patients stated that communicating with their health care providers and social circles helped ease the transition. The results highlighted that considering patient perspectives and having good patient–provider communication are important when considering future switching policy changes.