The Evidence Speaks Series is a recurring feature highlighting the latest in CHÉOS research. This series features summaries of select publications as well as in-depth features on the latest work from our investigators. In the early days of CHÉOS, the Centre had a series known as “The Evidence Speaks,” a monograph series to keep media and the research community up-to-date with CHÉOS’ current research results in the health outcomes field.
Wood DA, Lauck SB, Cairns JA, Humphries KH, Cook R, et al. The Vancouver 3M (Multidisciplinary, Multimodality, But Minimalist) Clinical Pathway Facilitates Safe Next-Day Discharge Home at Low-, Medium-, and High-Volume Transfemoral Transcatheter Aortic Valve Replacement Centers: The 3M TAVR Study. JACC Cardiovasc Interv. 2019 Mar;12(5):459-469.
Drs. Sandra Lauck and Karin Humphries are co-authors on a recent publication that further demonstrates the safety and efficacy of the Vancouver 3M Clinical Pathway, a structured approach to transfemoral transcatheter aortic valve replacement (TAVR) that focuses on next-day discharge. Transfemoral TAVR refers to a minimally invasive procedure to replace a failing aortic heart valve via an incision in the femoral artery of the leg (see inset). Though the Vancouver Pathway has been shown to be safe and effective in smaller studies and retrospective analyses, evidence from a multi-center, prospective 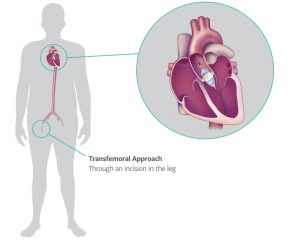 study was not available. To obtain this evidence, a large team of investigators from across Canada and the U.S. enrolled 13 centers of varying patient volume (low-, medium-, and high-volume) to implement the Vancouver Pathway for TAVR. The research team was primarily interested in all-cause death within 30 days of the procedure and the proportion of patients successfully discharged the day after the procedure. Secondary outcomes included hospital readmission, major bleeding or vascular complications, and need for repeated TAVR. Across 1,400 screened patients, 411 were enrolled. Most patients needed only minimal sedation (69 per cent) and 30 per cent needed no sedation. The procedure itself generally took between 30 and 60 minutes and most patients were in the surgical room for less than 2 hours. Next-day discharge was achieved in 80.1 per cent of patients and 89.5 per cent of patients were discharged within 2 days. Only 2.9 per cent of patients died or had a stroke within 30 days of the procedure. None of the primary or secondary outcomes were affected by hospital volume. The rate of next-day discharge was significantly higher than the highest reported rate in studies using other clinical pathways (23 per cent). Before enrolling in this study, 9 of the 13 study sites had never discharged a patient within 48 hours after TAVR. The rates of mortality, stroke, and secondary clinical outcomes (bleeding, readmission, etc.) was comparable to studies using other clinical pathways. This study adds further evidence to the case for using the Vancouver Pathway as the benchmark for standard of care in TAVR. The research team is planning to assess the potential cost-savings of this pathway and its impact on quality-of-life.
study was not available. To obtain this evidence, a large team of investigators from across Canada and the U.S. enrolled 13 centers of varying patient volume (low-, medium-, and high-volume) to implement the Vancouver Pathway for TAVR. The research team was primarily interested in all-cause death within 30 days of the procedure and the proportion of patients successfully discharged the day after the procedure. Secondary outcomes included hospital readmission, major bleeding or vascular complications, and need for repeated TAVR. Across 1,400 screened patients, 411 were enrolled. Most patients needed only minimal sedation (69 per cent) and 30 per cent needed no sedation. The procedure itself generally took between 30 and 60 minutes and most patients were in the surgical room for less than 2 hours. Next-day discharge was achieved in 80.1 per cent of patients and 89.5 per cent of patients were discharged within 2 days. Only 2.9 per cent of patients died or had a stroke within 30 days of the procedure. None of the primary or secondary outcomes were affected by hospital volume. The rate of next-day discharge was significantly higher than the highest reported rate in studies using other clinical pathways (23 per cent). Before enrolling in this study, 9 of the 13 study sites had never discharged a patient within 48 hours after TAVR. The rates of mortality, stroke, and secondary clinical outcomes (bleeding, readmission, etc.) was comparable to studies using other clinical pathways. This study adds further evidence to the case for using the Vancouver Pathway as the benchmark for standard of care in TAVR. The research team is planning to assess the potential cost-savings of this pathway and its impact on quality-of-life.
—
Hedden L, Lavergne MR, McGrail KM, Law MR, Bourgeault IL, McCracken R, Barer ML. Trends in Providing Out-of-Office, Urgent After-Hours, and On-Call Care in British Columbia. Ann Fam Med. 2019 Mar;17(2):116-124.
CHÉOS Scientist Dr. Rita McCracken’s newest publication looks at how provision of care by family physicians changed over a 6-year period with respect to care in non-office settings and after hours. Along with researchers from UBC, SFU, and the University of Ottawa, Dr. McCracken used administrative data from Population Data BC and MSP payment records for 2006–2012 to identify how often physicians were providing care in alternative locations and to quantify their participation in after-hours and on-call care. Alternative locations included patients’ homes, long-term care facilities, emergency departments, and acute-care hospitals. Data were analyzed according to whether a physician practiced in a metropolitan, urban, or rural setting. A physician’s patient population was also characterized, measured by the individual proportions of patients who were women, over the aged of 65, low socioeconomic status, and high morbidity. Over 6,500 physicians were included in the final analysis. Most physicians provided service in an alternative location and outside of office hours however participation declined over the 6-year study period. Care provided at alternative locations and after hours declined in all areas but rural physicians were more likely to provide alternative care than those in metropolitan areas. Female physicians and those older than 65 were less likely to provide care at other locations or after-hours. Provision of care at alternative locations was influenced by a physician’s patient population. For example, physicians with a higher proportion of chronically ill patients were more likely to provide care at hospitals and emergency departments. This analysis further confirms that existing incentives to expand care provision are ineffective and also highlights potential areas of significant challenge for accessing care in different areas of the province.
—
Bagshaw SM, Adhikari NKJ, Burns KEA, Friedrich JO, Bouchard J,…Dodek P, et al.; Canadian Critical Care Trials Group. Selection and Receipt of Kidney Replacement in Critically Ill Older Patients with AKI. Clin J Am Soc Nephrol. 2019 Mar:CJN.05530518.
Dr. Peter Dodek’s most recent publication, co-authored as part of his membership in the Canadian Clinical Care Trials Group, explores the factors, care process, and outcomes related to kidney replacement therapy and physicians’ willingness to offer replacement to older patients in the ICU with acute kidney injury (AKI). The research group designed an observation cohort study conducted at 16 ICU’s across Canada and recruited 499 ICU patients over the age of 65 with severe AKI. The study focused on whether or not patients received a kidney replacement and the willingness of the attending physician to offer replacement. Data were analyzed to determine the impact of these factors on 90-day mortality, rehospitalization, quality of life, and other outcomes. Forty-six per cent of patient received kidney replacement and clinicians reported willingness to offer kidney replacement in 72 per cent of patients. Ninety-day mortality was similar between people who did (50 per cent) and did not (51 per cent) receive kidney replacement. There were two distinct groups of patients for whom clinicians were not willing to provide kidney replacement: patients with a high likelihood of recovery and patients that were not likely to benefit from kidney replacement or for whom replacement was not part of their goals of care; mortality was high among the second group. Nine percent of patients for whom physicians were not willing to offer replacement received a kidney (12 patients); 75 per cent of this group died within 90 days. Age was associated with a lower likelihood of receiving kidney replacement. Quality of life was relatively low among patients who survived past 90 days but no difference was found between those who received kidney replacement and those who did not. This study highlights some of the nuances related to decision making about kidney replacement and may help frame discussions between patients, families, and care providers about kidney replacement in this population.