Our Clinical Research 101 series takes an in-depth look at key steps and tips for navigating the clinical research process. The tenth instalment in our Clinical Research 101 series is by Leslie Love, Senior Project Manager at CHÉOS. The following is a brief overview of regulatory inspections and how to prepare for them.
Ms. Love is a certified clinical research professional with over 20 years of experience in a variety of research settings. Her primary role is to provide project management support to CHÉOS and Canadian HIV Trials Network-supported investigators, as well as develop research training materials and programs. Ms. Love is one of many project managers who work for CHÉOS. The Centre’s project managers are experts in the regulatory, policy, budgeting, and implementation requirements for clinical research studies. If you would like to inquire about our services, please submit your request here.
Clinical Research 101 Series
What is a Regulatory Inspection?
All clinical research studies that test a new drug, or a licensed drug outside its intended use, must be submitted to and approved by Canada’s regulatory agency: the Health Products and Food Branch of Health Canada. (Clinical trials with Medical Devices are regulated under the Food and Drugs Act and the Medical Devices Regulations. We focus on drug studies here, but much of what is discussed applies to research in medical devices too.)
These studies are then subject to audits or inspections by the Clinical Trial Compliance Unit of Health Canada to ensure the study is being conducted according to the protocol and Good Clinical Practice (GCP)*. Inspectors assess whether a site complies with legal requirements in order to protect the rights, safety, and well-being of the study participants in clinical trials, and to ensure the integrity and accuracy of the data being collected in the study.
*As a reminder, Good Clinical Practice (GCP) is an international ethical and scientific quality standard for designing, recording and reporting trials that involve the participation of human subjects. Compliance with this standard provides public assurance that the rights, safety and well-being of trial subjects are protected, and that clinical trial data are credible.
What Will Inspectors Look for When They Perform an Inspection?
Inspectors review the study with reference to Part C, Division 5 of the Food and Drug Regulations: Drugs for Clinical Trials Involving Human Subjects. Specifically they look to ensure the study is conducted according to GCP and the methodology outlined in the approved study protocol. This not only includes verifying that the study protocol is being followed, but that those working on the study have been adequately and properly trained, that there is consistent, quality record keeping, that Standard Operating Procedures (SOPs) are in place, and that the site investigator (known as the Qualified Investigator) is providing appropriate medical supervision. (For more about the responsibilities of an investigator in a clinical trial, see this post from CHÉOS Project Manager Salima Jutha.)
In 2014–2015 there were 55 clinical sites inspected in Canada — only 41 were found to be compliant (Fig. 1). 457 observations were noted, primarily against requirements for Records, and System and Procedures.
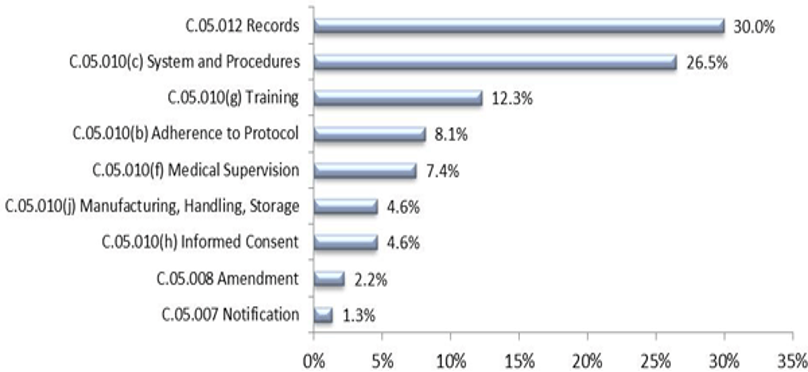
Figure 1: Sections of the Food and Drug Regulations (FDR) (Division 5 of Part C) most often cited, as a percentage of the total number of observations cited during GCP inspections across Canada in 2014-15, from www.canada.ca.
Examples of common observations:
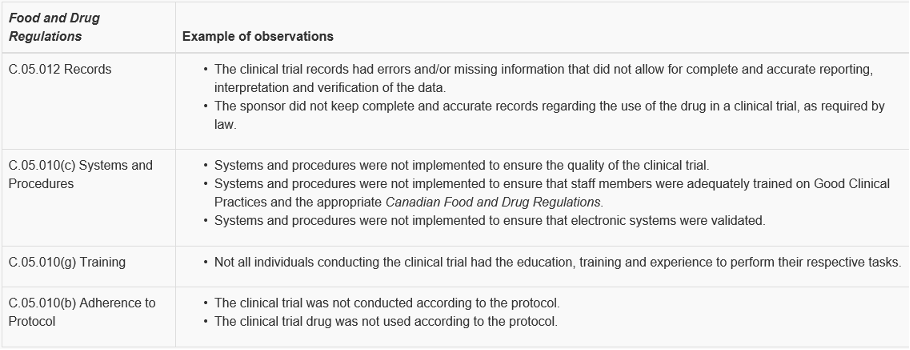
Adapted from: Health Canada Annual Inspection Summary Report 2014–15.
If Health Canada finds that a site is non-compliant (with GCP and/or the study protocol), the site will required to address the issues and the study could be put on hold at the site until the issues are addressed. In some, fortunately rare, circumstances, the study may be closed at the site, and the investigator is not able to further participate in clinical research.
How Can My Site be Compliant?
Trying to be continuously compliant with GCP regulations can often feel overwhelming. Many institutions have departments whose responsibility is to understand, interpret, and ensure their staff are following GCP regulations. Health Canada has produced a new document that provides guidance in the interpretation of the regulations. The final version is not yet available, but will be posted on the CHÉOS website when it is released. (Expected in the Spring 2019.)
In the meantime, what can an individual, or small site do to be prepared for an inspection?
Training:
- Ensure you have clinical research SOPs, and follow those SOPs. N2 Canada offers SOPs to member sites across Canada (see resource link below).
- Ensure you are trained on all aspects of the protocol as well as GCP. N2 can help with providing access to the appropriate training.
- Follow the protocol. Always. If you are unable to follow the protocol for any reason (called a protocol deviation), explicitly document the reason. A protocol deviation is absolutely allowed if there is a concern for participant safety but proper documentation is essential.
- Ensure you are completing study tasks that are within your ability and/or training. For example, only medical personnel should be doing physical exams or assessing adverse events. Health Canada requires all sites keep a Delegation Log that indicates who does what.
Systems and Procedures:
- You need to calibrate your equipment.
- Are your systems validated?
Records:
- Document, document, document. We have a saying in clinical research “if it’s not documented, it did not happen”.
Medical Supervision:
- The lead site investigator (or Qualified Investigator; QI) is expected to be up to date on study activities and pertinent developments in the study process, particularly as it relates to participant recruitment and safety.
- All adverse events must be reviewed by a physician.
If you have an industry or external sponsor, they are required to provide resources to ensure that study staff follow GCP. However, the sponsor cannot always be relied upon to help during a regulatory inspection.
If a site is selected for a regulatory inspection, CHÉOS can provide guidance on what to expect, and review the readiness of your site. Contact researchsupport@cheos.ubc.ca for more information.
Links to references and resources:
Health Canada Inspectorate Program –Annual Inspection Summary Report 2014-2015
Health Canada Food and Drugs Act and Regulations – Relevant Links
N2 Canada: Network of Networks



